Executive summary
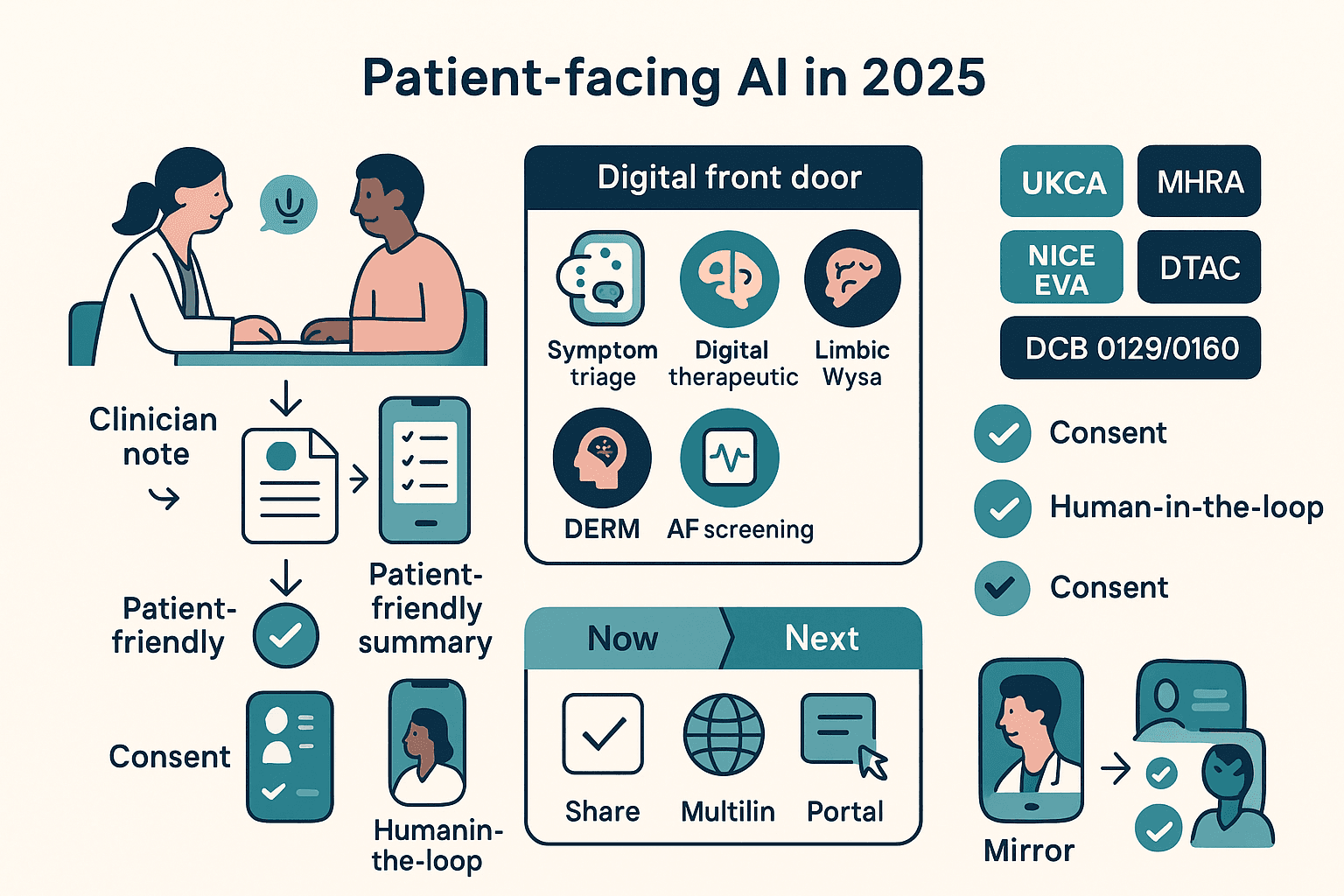
In 2025, patient-facing artificial intelligence has moved far beyond simple Q&A chatbots. The UK is now seeing the scaled adoption of regulated digital therapeutics and sophisticated intake tools, with tangible, NICE-recognised cost savings in primary care and a growing number of UKCA/MHRA-approved devices in areas like mental health triage and dermatology.
A new and exciting class of "consultation companion" is also arriving. Tools like Mirror by Aide Health are designed to empower patients by summarising their clinical visits in plain English and allowing them to query their own record afterwards. For the NHS, the immediate opportunity is to scale the use-cases that are already proven to work—such as Sleepio for insomnia, Limbic Access for talking therapies triage, and FibriCheck for AF screening—while developing clear "digital front door" standards to safely evaluate and adopt the next wave of innovation.
Where we are now: the UK patient-AI landscape (2025 snapshot)
- Symptom triage & guidance: Ada Health remains a well-known consumer symptom assessment tool, while platforms like AskFirst (by Sensely) are used in some NHS regions for online triage and access. These sit alongside the national NHS 111 online service, which focuses on safe routing to the right service, not definitive diagnosis.
- Mental health: Wysa is used to support patients in NHS Talking Therapies and is one of the first AI mental health apps to meet the DCB0129 clinical safety standard. Limbic Access holds a UKCA Class IIa mark for its role in streamlining intake and triage for common mental health disorders.
- Digital therapeutics: Sleepio, a digital therapeutic for insomnia, has been conditionally recommended by NICE as a cost-saving option for primary care.
- Dermatology AI: Skin Analytics' DERM is being deployed across multiple NHS sites, with NICE conditionally recommending the use of AI for skin lesion assessment while further evidence is gathered.
- Cardio self-screening: FibriCheck is a CE-marked application that allows for atrial fibrillation (AF) screening using the camera on a patient's smartphone or wearable.
New category: the consultation companion
A powerful new category of tool is emerging, focused on the patient's experience during and after a consultation. Mirror by Aide Health is an AI note-taker designed for patients, not clinicians. It listens during a consultation (with consent) and produces a plain-English summary of what was discussed, what to do next, and allows the patient to ask questions of their own record afterwards. It also supports secure sharing with carers and family members (Digital Health, Aide Health).
This matters because it directly combats the problem of information overload for patients, has the potential to improve recall and medication adherence, and could help to narrow health inequalities for those with limited health literacy.
What’s actually proven (and what’s promising)
Proven/endorsed
- Sleepio: NICE's Medtech Innovation Briefing (MTG70) concluded that Sleepio is a cost-saving intervention at £45 per person, leading to fewer GP appointments and hypnotic prescriptions compared to usual care.
- Wysa: Is in active use within NHS Talking Therapies and is a notable early leader in demonstrating compliance with the NHS's DCB0129 clinical safety standard.
- Limbic Access: Holds a UKCA Class IIa mark for its mental health triage tool and has published data on its diagnostic prediction accuracy in a real-world service.
- Skin Analytics (DERM): Has active NHS deployments, a body of peer-reviewed accuracy data, and a conditional green light from NICE under its evidence-generation pathway.
Promising/early
- Mirror by Aide Health: As a new category, these patient-owned summary tools require local assurance (DTAC, IG) and careful evaluation of their impact on adherence and safety outcomes before any large-scale deployment.
- Symptom checkers: While widely used by the public, their accuracy and safety vary. They are best used when coupled with clear clinical routing and unambiguous disclaimers.
How these tools fit the NHS “digital front door”
The adoption of these tools is being shaped by national policy. The NICE HTE/EVA pathways for digital front door and mental health tools are defining the evidence that commissioners need to see before scaling a new technology. In practice, the NHS App and regional programmes are already routing large volumes of patients via 111 online and local triage apps. For commissioners, the key questions to ask any vendor are about their UKCA/MHRA status, their DTAC pack, their clinical-safety cases (DCB0129/0160), and any signals of cost-effectiveness or ROI.
Mini case studies
| Tool | NICE/UKCA Status | Primary KPI |
|---|---|---|
| Sleepio | NICE MTG70 (cost-saving) | Completion rates, ISI score change, prescribing reduction |
| Wysa | DCB0129 compliant | Engagement, step-up/step-down rates, recovery scores |
| Limbic Access | UKCA Class IIa | Time-to-assessment, triage accuracy, waitlist movement |
| Skin Analytics (DERM) | NICE EVA | Time-to-decision, 2WW pathway optimisation |
| Mirror by Aide Health | Early adoption | Recall/adherence, complaint rates, safety events |
Risks, limits and how to mitigate them
- Over-trust & misdirection (symptom checkers): Mitigate by ensuring tools use provenance-first content and have clear, tested escalation rules to urgent care.
- Privacy & consent (consultation companions): This is non-negotiable. An explicit, documented consent process, a local DPIA, and ensuring patient ownership of their summaries are essential. Mirror positions itself as a patient-first tool to address this.
- Equity: Mitigate by ensuring tools meet accessibility standards, offer multilingual support where possible, and have offline alternatives. Outcomes should be evaluated by deprivation decile, not just service-wide averages.
What’s next: plausible futures (2026–2030)
- Patient-held “memory” becomes standard: Expect to see patient-friendly summaries automatically appearing in the NHS App, with features for family-sharing and medication safety prompts.
- Ambient triage + digital therapeutics: Intake tools like Limbic will be able to directly e-prescribe NICE-endorsed digital therapeutics like Sleepio, with the outcomes written back to the patient's record.
- Dermatology & AF at scale: AI triage for skin lesions (DERM) and phone-based AF screening (FibriCheck) will become embedded in routine community and primary care pathways.
- Smarter “front doors”: The NICE HTE/EVA frameworks will shape a national standard for safe and effective symptom-to-service routing, with a more conversational user experience converging across 111 online, GP websites, and ICS apps.
Buyer’s checklist for ICSs & providers
- Regulatory: UKCA/MHRA status; DCB0129/0160 clinical-safety cases; DTAC passed.
- Evidence: NICE guidance/EVA where applicable; published performance data and peer review.
- Data & IG: DPIA complete; clear consent flows; patient has control over their data.
- Economics: Clear KPIs (appointments avoided, time-to-decision), with agreed measurement windows.
- Equity: Accessibility standards met; a plan to monitor for differential outcomes.
FAQs
- Is Mirror by Aide Health a clinician scribe?
- No, it’s built for patients. It creates a plain-English record of a visit and allows them to ask questions of it afterwards.
- Which of these tools already have NICE support?
- Sleepio is formally recommended by NICE as a cost-saving option in primary care for insomnia. Other digital therapies and triage tools are in the NICE EVA pipeline.
- Are mental-health chatbots “approved” for NHS use?
- Wysa meets the NHS's DCB0129 clinical safety standard and is in use in NHS Talking Therapies. Limbic Access holds a UKCA Class IIa mark for its triage role.