Executive summary
Ambient voice technology (AVT), or the "AI scribe," has rapidly moved from a tool for reducing clinician documentation to a powerful new medium for patient engagement. The latest evolution is the generation of patient-facing outputs: real-time visit summaries, discharge instructions, and clinic letters written in plain, accessible English and even multiple languages. Platforms like Abridge and Nuance DAX Copilot are already deploying these features, and NHS sites are beginning to pilot AI-drafted clinic letters generated from ambient recordings (Digital Health, Abridge, Microsoft).
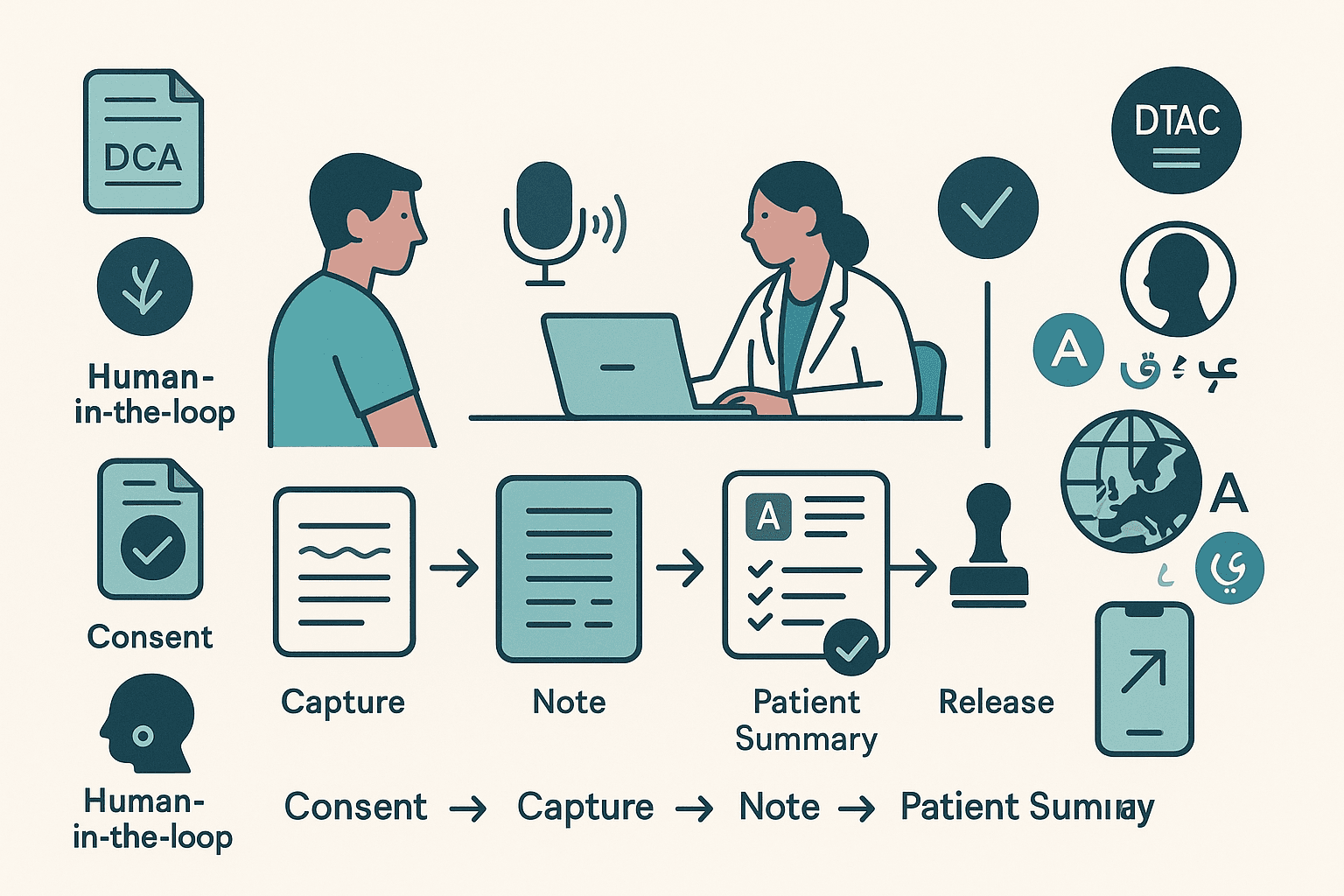
This shift matters because the evidence shows it can work. Studies have demonstrated that AI can significantly improve the readability of complex discharge information, and separate research on patient access to visit notes (the "OpenNotes" movement) has linked it to better medication adherence and patient understanding (ACP Journals, JAMA Network, PMC). However, for UK adopters, this innovation must be navigated through a clear governance framework, including NHS England’s ambient scribe guidance, the DTAC, and clinical safety standards, while the EU AI Act introduces new duties for deployers around consent and oversight.
What we mean by “patient-facing” ambient voice
This represents a move from clinician-only notes to co-produced artefacts of the consultation. It’s about creating simplified visit summaries that clearly outline "what to do next," any medication changes, and the agreed follow-up plan, which can then be delivered to the patient's portal or as a letter. The typical workflow is: capture → transcript → structured clinical note → patient-friendly summary → clinician review → release to patient.
The tools landscape (2025 snapshot)
- Abridge: A leader in this space, Abridge now generates real-time Patient Visit Summaries alongside its clinical notes, with a clear breakdown of the plan and instructions. It is also actively evaluating the impact of this feature with OpenNotes.
- Nuance DAX Copilot: The ambient capture solution from Nuance/Microsoft includes functionality to generate patient-friendly after-visit summaries directly from the approved clinical documentation.
- AWS HealthScribe: Amazon's generative AI service for healthcare includes templates for creating patient-centred sections, demonstrating that this is becoming a standard feature for modern clinical AI platforms.
- NHS pilots (UK): The GOSH-led multi-site AVT trials, which included the use of Tortus, have explored using the technology to draft both clinical notes and the letters sent to patients after a clinician has signed them off.
The benefits (with evidence you can cite)
- Improved comprehension: A study in JAMA Network Open found that LLMs could translate complex, jargon-filled discharge summaries into plain language with significantly higher readability scores—though it stressed that clinician review remains essential for safety.
- Better activation & adherence: The extensive body of research from the OpenNotes movement has consistently linked patient access to their own visit notes with better medication adherence, a deeper understanding of their care plan, and increased trust.
- Enhanced experience & efficiency: Health systems in the US, like Sutter Health using Abridge, have reported that providing patient-friendly summaries improves the patient experience and makes instructions more readily available after the visit.
What’s emerging next (near-term trends)
- Multilingual, same-day discharge information: The ability to draft summaries in multiple languages, which can then be quality-checked by a human translator, promises to cut significant delays.
- Real-time interpretation overlays: Pilots are underway to use this technology to provide real-time interpretation during consultations, reducing friction for patients with limited English proficiency.
- Structured “care-plan” summaries: Expect to see these summaries pushed directly to patient portals as interactive checklists, medication countdowns, and follow-up reminders.
- Patient-message assistance: The same technology is being used to draft replies to inbound patient portal messages, which a clinician can then review, edit, and send, reducing administrative workload.
Risks & design challenges
- Consent for recording: This is a critical hurdle. Patients need absolute clarity on what is being captured, who will review it, where it is stored, and how they can opt-out. Evidence from JAMA suggests that a multi-modal consent process (e.g., a pre-visit notice, a clear in-room script, and a portal reminder) is more effective than a quick verbal check.
- Secondary data use: The datasets generated by ambient scribing are incredibly valuable for AI model training. Transparency and clear limits on this secondary use are essential for maintaining patient trust.
- Accuracy/omissions: The process of translating technical notes into plain English can lead to the omission of crucial nuance. Mandatory clinical sign-off on every patient-facing output is a non-negotiable safety step.
- Equity & language: Automated translation must incorporate a human review step for any safety-critical content, such as medication instructions.
Regulatory & assurance map (UK/EU)
- NHS England AVT guidance (April 2025): This is the foundational document for UK adopters. It sets out the core principles for adoption, including the need for transparency with patients and clear "human-in-the-loop" expectations.
- DTAC + DCB0129/0160: Any solution that writes into a patient record or outputs clinical instructions must meet the procurement baseline of the DTAC and be supported by the DCB clinical safety standards.
- EU AI Act: For organisations operating in or selling into Europe, the AI Act introduces explicit duties for deployers of "high-risk" AI systems (which can include clinical tools). These include ensuring AI literacy for users, maintaining detailed logs, and guaranteeing human oversight.
Implementation blueprint (90-day pilot)
- Define the patient artefact: Decide what you will produce (e.g., an after-visit summary for a specific outpatient clinic), the target reading age, and the required languages.
- Design the consent pathway: Create a layered, documented consent process with clear pre-visit notices, an in-room script, and an easy opt-out mechanism.
- Establish safety netting: Mandate a clinician review and sign-off for every single patient-facing output. Create red-flag templates for high-risk advice. For translations, design a human quality-check workflow.
- Define your metrics: Track the time-to-letter, readability scores, patient comprehension (via surveys), re-attendance calls for clarification, and any medication adherence proxies.
- Assemble your assurance pack: Ensure your chosen vendor provides their DTAC artefacts and DCB safety case, and complete your local DPIA, all aligned to the NHSE AVT guidance.
FAQs
- Is this just for clinicians?
- No. Major vendors like Abridge and Microsoft (Nuance) now explicitly support the generation of patient-facing summaries and letters, always with clinician approval as the final step.
- Does AI replace discharge nurses or the need for counselling?
- No. The studies emphasise the gains in the readability and speed of producing written materials. They do not replace the need for human review for accuracy and safety, nor the vital role of in-person counselling and education.
- How do we handle patient consent properly?
- Use a layered and documented consent process that includes clear opt-out routes and a simple explanation of how the data will be used. Evidence shows this approach improves patient acceptance.
- What about different languages?
- The best-practice model is to combine an instant AI draft translation with a rapid human quality assurance check for any safety-critical content like medication instructions.