Executive summary
Sustainable growth in health AI is not about downloads or pilots; it's about becoming an indispensable part of a clinician's daily workflow. The most successful platforms achieve this by landing a critical task, then compounding their advantage through network effects, demonstrable compliance, and proven clinical or operational outcomes.
The evidence from the market is clear. Doximity built a dominant network of over 80% of US physicians by starting with a simple, high-utility wedge. Abridge is scaling across hundreds of health systems by integrating deeply into EHR workflows and proving a clear return on investment. OpenEvidence has achieved explosive growth by combining a free, high-quality product with a powerful CME/CPD habit loop. And in the UK, adoption accelerates when tools align with NHS procurement and safety standards (DTAC, DCB, NICE) and can demonstrate tangible productivity gains, such as the staff-time savings modelled in recent ambient AI trials.
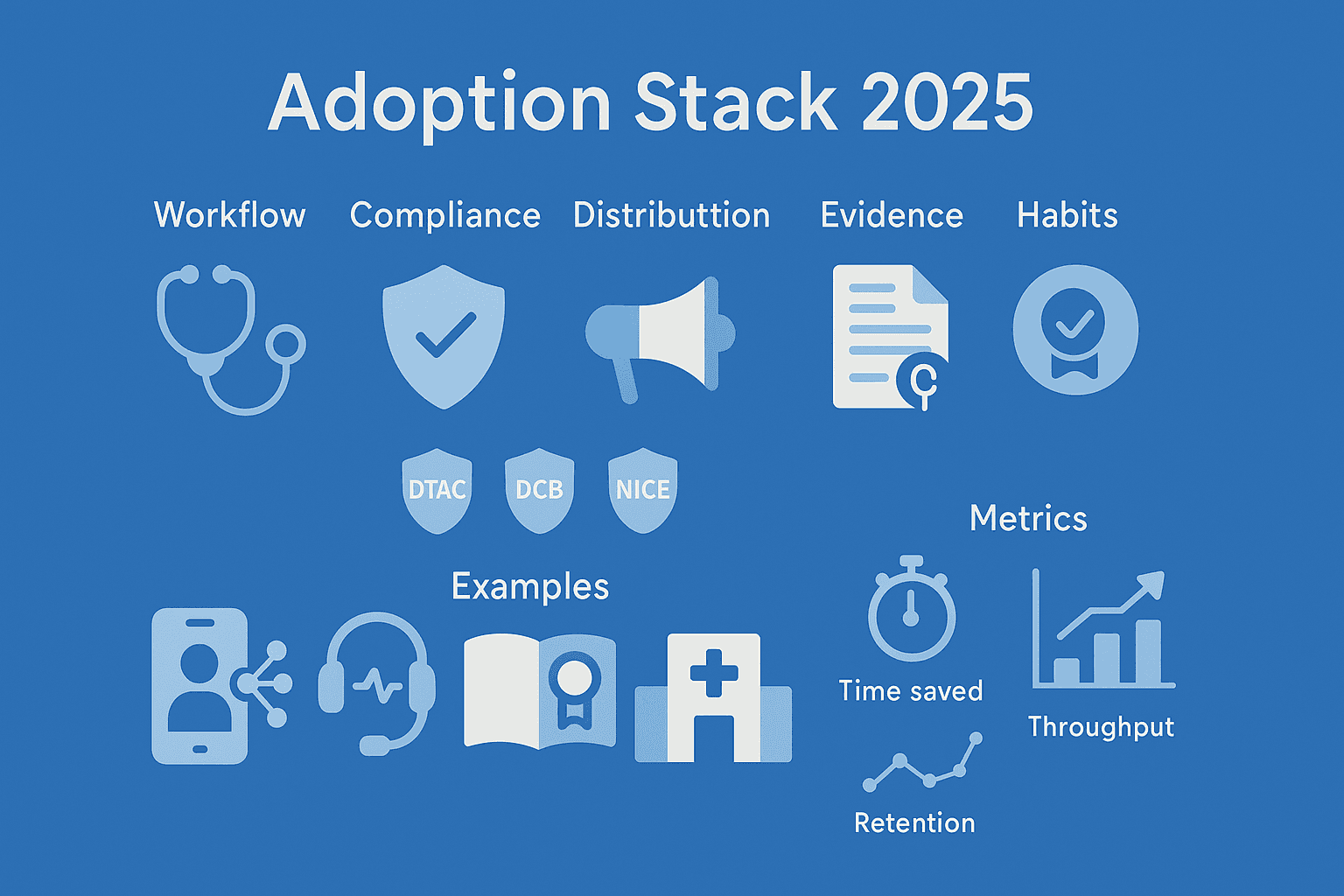
The adoption stack (five levers you must plan up-front)
- Land a daily workflow: Solve one, undeniable, painful step in a clinician's day—note-taking, secure messaging, searching, or referrals.
- Trust & compliance by design: Build in privacy, audit trails, and citations from day one. In the UK, this means aligning with DTAC, MHRA, and NICE pathways.
- Distribution channels beyond sales: Utilise EHR marketplaces, app stores, professional bodies, and institutional licenses to reach users.
- The evidence flywheel: Publish before-and-after metrics and empower your clinical champions to create peer-to-peer case studies.
- Habit loops: Reward continued use with features like CME/CPD credits, shareable templates, team analytics, and content personalisation.
Case studies (what scaled—and why)
Doximity: utility wedge → network effects → multi-product platform
Doximity’s strategy is a masterclass in building a network. They began by offering free, privacy-safe utilities (like secure faxing and the Dialer telehealth tool) that solved a daily problem for US doctors. During the telehealth surge, over 45% of physicians with Medicare telemedicine claims used Doximity Dialer, cementing it as a daily habit. This created a powerful network effect, which they leveraged to expand into news, hiring, and pharmaceutical marketing. The lesson: land with a free, indispensable utility, verify user identities to build a trusted community, and then expand your offering.
Abridge: enterprise ambient AI via EHR routes and ROI narrative
Abridge has scaled rapidly by focusing on the enterprise market and integrating deeply with major EHRs. Now used across more than 200 health systems, with organisations like UPMC rolling it out enterprise-wide, its success is built on a clear ROI narrative. By attaching to existing systems, publishing data on time savings and throughput gains, and winning over clinicians, it has become a leader in the ambient AI space.
OpenEvidence: freemium + CME → habit formation for point-of-care Q&A
OpenEvidence has seen explosive growth by removing friction and rewarding usage. It offers its core AI-powered medical reference tool for free to verified healthcare professionals. Crucially, it has integrated a free CME/CPD feature that turns the everyday act of asking a clinical question into an accredited learning event. This creates a powerful habit loop, encouraging clinicians to return to the platform daily.
Nuance DAX Copilot: leverage an installed base
Nuance (a Microsoft company) accelerated the adoption of its DAX Copilot ambient AI by layering it on top of the massive existing footprint of its Dragon Medical dictation software, used by over 600,000 clinicians. The lesson is simple: if you have an incumbent asset—whether it's an SSO integration or a widely used pager app—build on it, not around it.
Education on-ramp (SimConverse / Geeky Medics)
Another powerful growth route is to start in education. AI communication and OSCE simulation tools like SimConverse (used by BMJ OnExamination) and Geeky Medics are being adopted by UK universities and training programmes. This classic institution-first strategy seeds the future user base, building habits and brand loyalty with the next generation of clinicians before they even qualify.
NHS adoption realities (what to evidence and when)
In the UK, buyers move when a tool can prove it solves one of two core problems: productivity or safety. The headlines from the HSJ about ambient AI in emergency departments—modelling ~£1bn in staff-time savings and a ~13% increase in patients seen—is the kind of evidence that drives adoption. To get there, your product must be built on a foundation of assurance: a passed DTAC, a robust DCB0129/0160 safety case, and, where applicable, alignment with a NICE EVA pathway.
The go-to-market (GTM) blueprint (90–180 days)
- Phase A — Find your daily wedge: Shadow users and quantify a single painful step. Ship a narrow, free utility with an explicit privacy posture.
- Phase B — Instrument & publish: Pre-register 2-3 key metrics (e.g., minutes saved). Run a stepped-wedge pilot and release a short, citable report.
- Phase C — Distribution beyond sales: Explore EHR marketplace pathways and institutional licenses with education partners.
- Phase D — Habit & monetisation: Add a CME/CPD credit loop. Introduce team analytics.
Common Failure Modes
- Pilot purgatory: Avoid getting stuck in endless pilots by pre-registering your endpoints and having a clear date for a public read-out.
- Compliance afterthought: Treat your DTAC and DCB safety case as a "sprint zero" deliverable, not something to do later.
- No “one-minute win”: If your product's value only appears after months of use, you will struggle. Ship a feature that delivers a delightful, time-saving win on first use.
Metrics that predict scale
- Activation: Percentage of invited clinicians completing their first critical action within 24–48 hours.
- Time-to-value: The median number of minutes saved on day one and in week one.
- Habit: 7-day and 30-day retention rates; frequency of CME/CPD crediting.
- Trust: Percentage of answers where a user clicks through to the cited source (for RAG tools).
FAQs
- Do I need “AI” in my pitch?
- No. Sell the workflow outcome (e.g., "ten minutes back per consultation") and show the evidence and citations that prove it's safe.
- Should I start with consumers or institutions?
- In healthcare, institutional routes (via EHRs, universities, or NHS organisations) often provide a more durable path to adoption than purely consumer-focused plays.
- What about network effects?
- They are real and powerful in clinician networks, as Doximity proves. But they only kick in after you have nailed a daily, high-utility workflow.
Advisory note
insights by iatroX
iatroX offers consulting, advisory and go-to-market strategy services for AI companies and health platforms—led by Dr Kola Tytler, with over a decade of experience scaling lean products to millions of users. Engagements span proposition design, evidence and ROI frameworks, NHS-ready assurance, and growth playbooks tailored to clinical workflows. Enquire via iatroX Insights.