Executive summary
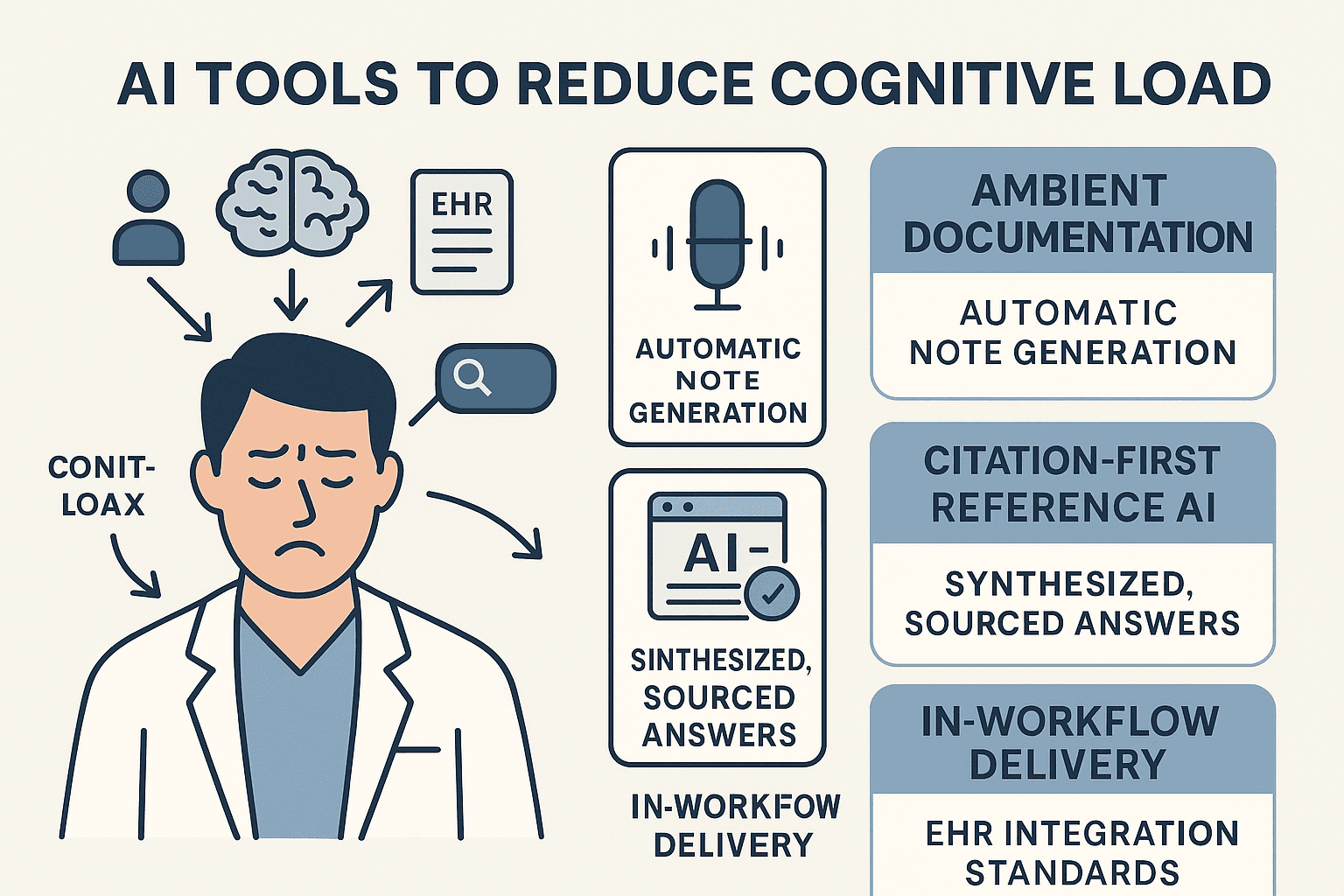
The modern clinical workday is defined by a heavy cognitive load. The frequent task-switching and administrative burden associated with Electronic Health Records (EHRs) are measurably linked to clinician stress and burnout (PMC, medinform.jmir.org). The most effective new artificial intelligence tools are those designed to directly combat this problem.
In 2025, the solutions fall into three main categories: (1) ambient documentation tools like Tortus and Microsoft Dragon Copilot/DAX that reduce administrative work; (2) citation-first reference AI like the UK-centric iatroX, EBSCO's Dyna AI, and OpenEvidence that provide fast answers without "tab-hopping"; and (3) in-workflow delivery standards like SMART on FHIR and CDS Hooks that bring these tools directly to the point of care. For the UK, this adoption is now supported by formal NHS England guidance on AI scribes, making it a key strategic priority (NHS England, hsj.co.uk).
The cognitive-load tax in modern clinical work
"Cognitive load" is the total amount of mental effort being used in your working memory. Systematic reviews have consistently associated higher cognitive load from EHR use and information fragmentation with clinician burnout (PMC). Every time you switch context—from the patient, to the EHR, to a separate browser tab, to a login screen, and back—you pay a "switching cost." Audit-log studies have shown that tasks performed immediately after a switch require more cognitive effort and are more prone to error. Reducing these switches is, therefore, a critical patient safety and workforce issue (ScienceDirect).
Tool category A — Ambient documentation to reclaim attention
The aim: fewer clicks, fewer windows, more headspace for patients.
Ambient documentation, or AI scribes, are designed to listen to the clinician-patient conversation and automatically generate structured notes, letters, and summaries. NHS England's 2025 guidance on AI-enabled ambient scribing has created a formal pathway for the safe adoption of these tools.
- Tortus (ED pilots): The impact of this technology has been highlighted by a large-scale NHS trial in emergency departments. As reported by HSJ, the study modelled a potential ~£834m in national staff-time savings and, crucially, a 13% increase in the number of patients seen, demonstrating a tangible return in throughput.
- Microsoft Dragon Copilot / Nuance DAX: This platform integrates ambient AI (DAX) with its established dictation tool (Dragon Medical One). Early studies show significant gains in provider experience and reduced documentation time, with Microsoft positioning it as an enterprise-grade solution for automated notes and letters.
These tools reduce cognitive load by shrinking the time spent on documentation and eliminating the jarring "mode shift" between engaging with a patient and then typing up the encounter.
Tool category B — Citation-first clinical reference AI to cut search fatigue
The aim: faster, trustworthy answers without multi-tab hunts.
This new generation of AI tools uses Retrieval-Augmented Generation (RAG) to provide a single, synthesised answer from a library of trusted sources, rather than making you hunt through a list of links.
- iatroX (UK-centric): A free clinical assistant designed for UK practice. Its Ask iatroX feature provides conversational answers grounded in authoritative UK-accepted guidance and peer-reviewed research, with clear citations. It also integrates a Quiz engine with spaced repetition, keeping learning and look-ups in one place.
- Dyna AI (EBSCO): A RAG-based assistant layered on top of the comprehensive DynaMed and DynaMedex databases. It is designed to surface cited evidence in-workflow and is now available to individual subscribers.
- OpenEvidence: A powerful evidence-synthesis tool, free for verified healthcare professionals, that excels at answering complex questions by referencing the latest medical literature.
These tools reduce cognitive load by collapsing the entire "search-synthesise-document" loop into a single, verifiable step.
Tool category C — Deliver it in-workflow (SSO + standards)
The aim: answers appear where you work, not in another app.
The final piece of the puzzle is integration. The best tool in the world is useless if it's too difficult to access.
- NHS Single Sign-On (OIDC): The use of NHS login and NHSmail single sign-on (SSO) is critical for reducing authentication friction, allowing clinicians to access approved services with one click.
- SMART on FHIR + CDS Hooks: These are the open standards that allow new tools to be safely embedded within your EHR. SMART on FHIR lets you launch an app from the patient record, while CDS Hooks enables proactive "cards" to appear with contextual suggestions (e.g., a dosing reminder) at the exact moment you're making a decision.
This layer reduces load by keeping your attention in a single surface and eliminating the copy-paste errors and login friction that fragment your working memory.
Fit-for-purpose selection: match pain-points to tools
- If documentation is the bottleneck: Pilot an ambient scribe (like Tortus or Dragon Copilot/DAX) under the official NHS England guidance. Measure your "pajama time" (after-hours EHR work) and time-to-note completion.
- If knowledge hunting drains time: Deploy a citation-first reference AI (like iatroX, Dyna AI, or OpenEvidence). Measure your time-to-answer, the click-through rate on citations (a proxy for trust), and any reduction in repeat queries.
- If context switching is rampant: Prioritise tools that integrate via NHS SSO and have a clear roadmap for SMART on FHIR/CDS Hooks.
Measurement & governance (checklist)
- Core KPIs: Time-to-note, time-with-patient, number of attention switches per session (from EHR audit logs), time-to-answer, and user-reported workload (e.g., via the NASA-TLX index).
- Safety & assurance: Follow the NHSE AI scribe guidance. Document your clinical oversight process. Prefer citation-first engines. Ensure any SSO implementations meet NHS OIDC guidance.
One-week pilot blueprint
- Day 0: Baseline your metrics. How many minutes do you spend on notes per clinic? How many times do you switch tabs to find an answer?
- Days 1–3: Introduce one ambient tool and one reference AI (iatroX, Dyna AI, or OpenEvidence). Train your pilot group on safe prompt patterns and the "verify citations" rule.
- Days 4–5: Enable SSO or EHR launch features where available. Capture user feedback and log any safety incidents or near-misses.
- End of week: Compare your KPIs. Keep only the interventions that demonstrably reduce your cognitive load and task-switching without compromising safety.
FAQs
- Do ambient scribes really save time?
- Yes. Controlled studies are showing significant gains in provider experience, and the large-scale UK ED pilots reported modelled time savings and a 13% throughput uplift. You must validate these claims in your own local setting.
- Why does a "citation-first" reference AI matter?
- It shortens your search time while preserving provenance. This directly tackles the "fear of error" barrier by allowing you to trust and verify, which is a key principle of iatroX, Dyna AI, and OpenEvidence.
- Is integration via SMART/CDS Hooks worth the hassle?
- Yes. The evidence shows that these standards reduce context switching and that proactive prompts can significantly increase the use of safety-critical apps within the workflow.